Case History
The patients, an eighty-five year old medically compromised male, with quadruple by- pass surgery (1990), and recently treated for a melanoma. Currently on Warfarin (anticoagulant), Cardiprin (aspirin), Crestor (statin), Physiotems (anti-hypertensive), Prazosin (alpha blocker, vasodilator) Micardis (anti-hypertensive), Digoxin (for heart rhythm disorders)
As a result of polypharmacy (taking of 3 or more pharmaceuticals), a liquid (saliva-like) is produced in the mouth, with a pH as low as 5.0-5.8 (highly acidic); compared to moderately acidic saliva pH 6.0-6.6 and healthy saliva pH 6.8-7.8. The buffering action of saliva is disrupted in these patients, the saliva produced, is a liquid with no buffering ability, and is in fact, a source of high acidity (pH 5.0-5.8), which usually can’t protect teeth surfaces effectively; this level of acidity in the mouth favours demineralisation and/or increasing colonisation by acidophilic bacteria. That is why we see rampant caries in this patient and other elderly patients compromised by polypharmacy.

OPG 03/02/2015
Note a hint of caries on the distal of 37 and a large carious lesion on the mesial of tooth 17.
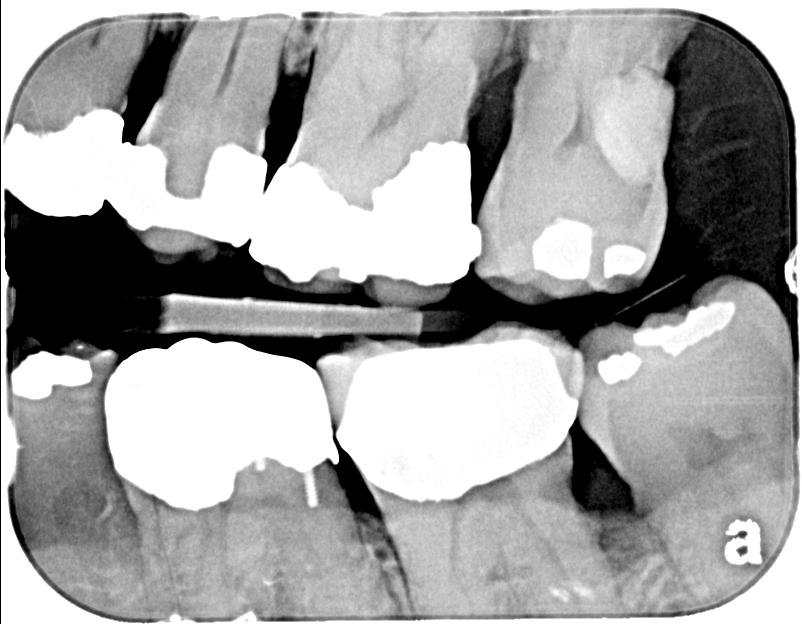
Bitewing radiograph (04/02/15) shows an area of translucency on the distal of 37, below the large restoration.
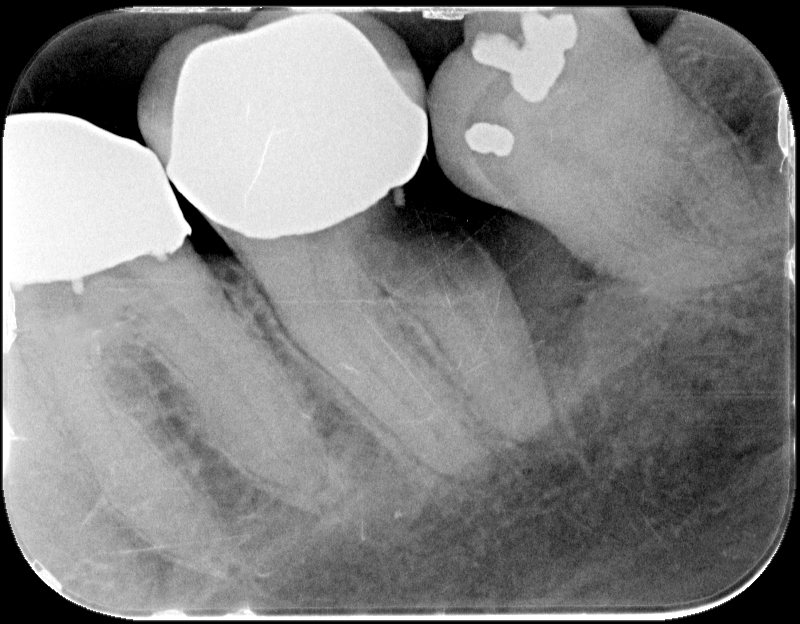
Periapical radiograph 14/06/2017 of 37, as a result of poor oral hygiene and dysfunctional saliva due to polypharmacy, shows very rapid caries progression from initial radiograph above date 04/02/2015
Tooth 37 17/10/2017; the patient was unable to maintain his oral hygiene and also because of the medical history it was decided to extract 37. With this in mind a consultation was held with the patient’s GP on how to best to manage the extraction given his dependence on anti-coagulants, and past difficulty in controlling bleeding after surgery. It was suggested that the patient be taken off Warfarin for at least 2 days before the surgery to manage the bleeding. His G.P agreed but insisted on maintaining some form of anticoagulant and prescribed Clexane to be taken on the day of the surgery. The tooth was extracted without complications, Spongestan placed in the wound and the socket sutured. The patient was not dismissed until the bleeding stopped and the wound was stable.
That night the wound began to bleed at around 7 pm continuing until 7am the next day (17/10/2017). He tried to arrest the bleeding by putting biting pressure on the wound with a gauze swab. The patient by his own accord discontinued the Clexane; after having bled all night and consulting with his GP in the morning, he was prescribed aspirin for that day and advised to recommence warfarin the next day which he did. Friday October 20, 2017; sutures were removed healing was progressing and Alvogyl placed in the socket.
Tooth 17 08/05/2018,was grossly decayed and would, under normal conditions, have been extracted; however, due to his history of abnormal bleeding even after packing the tooth socket and suturing, and the insistence of his GP to continue anti-coagulants before surgery, an alternative treatment was required. The crown was sectioned just above the gingiva and the remaining root stumps treated with AgF and SnF2 (CSDS).

22/10/2018, on examination after seven months, the tooth was asymptomatic; there was a lightening of the black layer formed after initial treatment on the root stumps especially on the mesio-buccal root; indicating caries progression, AgF and SnF2 were re-applied. The patient will be re-examined in 4 to 6 months when the root stumps will be re-assessed.
Reproduced with the kind permission of Dr David Sheen AM BDS (Usyd MHP (UNSW) FICD and Dr. Robert Lilia BDent(Hons BEdu (USyd) Lyons Dental, Russell Lea, NSW.